“The best position to kill a patient in, from an airway perspective, is flat on their back.”
-Rich Levitan – @airwaycam
This is one of the most important concepts in emergency airway management. Rich knows this better than anyone, having examined 20 cadaveric airways per month for the past 16 years in addition to clinical research. He coined the term “coffin position” to describe the detriment of having your patient supine. Cannot Oxygenate Face Flat in Neutral position. There are a few reasons this is true and it is important to understand them. Not only will it help improve patient outcomes but it will make you better at managing airways.
this better than anyone, having examined 20 cadaveric airways per month for the past 16 years in addition to clinical research. He coined the term “coffin position” to describe the detriment of having your patient supine. Cannot Oxygenate Face Flat in Neutral position. There are a few reasons this is true and it is important to understand them. Not only will it help improve patient outcomes but it will make you better at managing airways.
The Upper Airway
When we talk about airway management we are talking about the upper airway. Barring any severe trauma or pathophysiology, the airway south of the glottic opening is intrinsically patent. We are really only worried about the passageway above the glottis which is made up of soft tissues that do not have spontaneous patency. Normally, patency is maintained by muscles controlled consciously and unconsciously. But when patients are obtunded or sedated they lose the ability to maintain upper airway patency.


Bad things happen to the lungs when a patient as lying flat. It becomes much more difficult to fully recruit lung tissue. This is due to a number of factors and is much more profound in obese patients. The abdominal contents are no longer held off the diaphragm by gravity. They move upward and often push on the diaphragm preventing it from contracting fully. This also decreases the amount of thoracic space the lungs have to expand in. The net result is decreased amounts of usable lung tissue, lower functional residual capacity, and more difficulty recruiting alveoli. In addition, the obese have weight from fat which puts pressure on the chest and abdomen preventing lung expansion and contributing to the abdominal component of supine positioning. Obese patients desaturate significantly faster than average sized patients, mainly for this reason.
The Stomach
RSI is a technique that was designed with the stomach in mind, not the lungs. This is very important as it highlights one of the most detrimental complications during airway management, regurgitation. Vomiting can be active or passive. In an RSI scenario it is often passive as paralytics are given to help prevent it. However, active or passive vomiting can occur at any time during the airway management process. It is further encouraged by poor bag-valve-mask technique which insufflates the stomach with air. It is imperative to try to minimize the potential for regurgitation as much as possible.
Intubation
The end goal of any airway scenario is to secure the airway in the most appropriate means. This is frequently through endotracheal intubation. In the emergency setting, I believe the most frequently neglected aspect of this process is positioning. Proper patient positioning is probably THE MOST IMPORTANT factor that contributes to obtaining an adequate view of the cords. Not surprisingly, the worst position a patient can be in for this is flat on their back.
The Solution
All of the problems discussed above can be drastically improved by properly positioning your patient. This goes for ANY airway scenario whether you are setting up to intubate or doing procedural sedation. These techniques will work in the vast majority of patients.
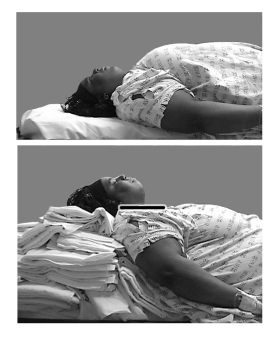
This method involves aligning the external auditory meatus with the sternal notch in the horizontal plane. If your patient is supine you are essentially elevating the head higher than the surface of the bed. This is to get the patient into the more natural airway position as was discussed earlier. It is easily accomplished by placing a pillow or towels under the occiput. Obese patients require more padding, or ramping. In kids, obtaining the position may require elevating the shoulders instead.

2. Sit your patient UP!
If you can only take one thing away from this post it is this: sit your patient up. This goes for any type of airway management and post-intubation situation. If the airway is at all compromised, sit them up. There are quite a few reasons to do this and really no downfalls.
In the upright position the lungs are able to expand more fully. This increases the functional residual capacity and improves oxygenation. This is the reason that intubated patients should usually be upright post-intubation; it will maximize their lung recruitment and ventilation. It also aids in oxygenation prior to intubation.
When patients are upright their tongues are not as prone to falling posterior. Combined with the ear-to-sternal notch position an upright patient will have a more spontaneously patent airway than a supine patient.
The upright position is likely to decrease the chances of regurgitation and aspiration. This is simple gravity but also is due to decreased pressure on the stomach and improved bag-valve-mask mechanics.
BVM use will be easier and more effective in the upright position. The airway is maintained more patent thus allowing better ventilation and less gastric insufflation.
Airway views during intubation are better with the patient sitting upright at 30 degrees or more. This is due to better alignment of airway structures and less force being required to displace the soft tissues.
3. Perform a jaw thrust
A jaw thrust is the most effective way of maintain airway patency non-invasively. Simply doing a head-tilt, chin lift does not completely displace the tongue from the posterior pharynx. If a patient is experiencing anatomical airway obstruction a jaw-thrust is likely to resolve it by lifting the tongue and creating a pathway for ventilation. It is important to maintain a jaw thrust in any patient being BVM ventilated, not controlling their own airway, and during the apneic period of RSI. When using apneic oxygenation (which should be used during any RSI) the airway must remain patent via jaw thrust during the apneic period.
The bottom line: patients with a compromised airway should be positioned upright in the ear-to-sternal notch position. Use a jaw thrust to resolve anatomical airway obstruction.
Like us on Facebook!
Questions, comments, feedback?
theresusroom@gmail.com
@amerelman on twitter
References:
- Khandelwal, N, et al. “Head-Elevated Patient Positioning Decreases Complications of Emergent Tracheal Intubation in the Ward and Intensive Care Unit.” Anesthesia and Analgesia 122.4 (2016): 1101-107.
- Levitan, Richard. Fundamentals of Airway Management. 3rd ed. Irving: Emergency Medicine Residents Association, 2015. Print.
- Weingart, Scott, and Levitan, Richard. “Preoxygenation and Prevention of Desaturation During Emergency Airway Management.” Annals of Emergency Medicine (2011): 165-75.
[…] first step to good BVM technique is properly positioning the patient. See my last post here for information on that […]
LikeLike
Thoughts on using this upright or 30 degree technique during CPR. I’ve see the advantages of sitting patients upright for many respiratory issues, but never considered it feasible to attempt any elevation during a full code.
LikeLike
Great question! There is mounting evidence that head up CPR may improve cerebral and coronary blood flow. It may be a win-win! I have used the Lucas with head up positioning without issue. See these links:
http://www.ncbi.nlm.nih.gov/m/pubmed/26905388/
http://circ.ahajournals.org/content/130/Suppl_2/A88
LikeLike
[…] Blair C sent me a great link for the airway anatomy and positioning (thanks […]
LikeLike
[…] * airway anatomy and positioning […]
LikeLike
[…] The Resus Room US: Airway anatomy and how we make it worse […]
LikeLike